A woman sat in the waiting room of our clinic; her eyes fixed on the floor. She wasn’t there for her own treatment, but rather to accompany her daughter who was having a different procedure.
During our customary conversations with patients in the lounge, she was asked if she needed any assistance. She spoke silently, eyes vacant, and eventually shared that she had received a diagnosis of macular degeneration at another clinic. However, she had received no information or guidance on how to manage her condition.
As we talked, she began to open up about her fears and concerns for the future. She had so many questions about macular degeneration, and yet had received no answers or context. It was clear that she needed help.
So, delving deeper, we discussed the different types of macular degeneration, the meaning of her diagnosis, and the available treatment strategies.
By the end of our conversation, the woman’s demeanour had changed. She was no longer staring into the distance, but sat upright and present, with a renewed understanding of her diagnosis.
That conversation inspired this article — to help this woman and many others like her who are living with macular degeneration.
Here, we will provide the answers for her 5 main questions about macular degeneration, including:
- What is macular degeneration, and how will it affect my vision?
- What are the early signs and symptoms of macular degeneration?
- How quickly can macular degeneration progress after diagnosis?
- What are the treatment and management options available?
- Are there any dietary or lifestyle modifications that can help manage or prevent macular degeneration?
These five points will help you navigate the most important question: how fast does macular degeneration set in and what is your prognosis?
With the right information and guidance, people with this diagnosis can continue to live full and meaningful lives. But it’s important to understand that early intervention is key.
Question 1
What is macular degeneration, and how will it affect my vision?
We understand how concerning it can be to receive a diagnosis for this sight-threatening eye condition. While there is currently no cure for macular degeneration, there are several treatment options available to help slow its progression and maintain as much of your vision as possible. And with the advancement of newer and more sophisticated technologies, managing macular degeneration has become much more effective than in the past.
Macular degeneration is a common eye condition that can cause blurry or distorted vision by damaging the part of your eye responsible for seeing details, called the macula.
It’s important to distinguish the two types of macular degeneration: dry and wet:
- The dry form usually progresses slowly over a period of years — when tissue in the macula thins and loses cells responsible for vision.
- The wet form, on the other hand, can cause rapid and severe vision loss — when irregular blood vessels grow and fluid leaks into the macula.
While some individuals may experience a slow loss of central vision, others may have trouble reading, seeing details or recognizing faces. And in severe cases, there may be a significant blind spot or distortion in the centre of the visual field — as you can see in the above comparison.
Question 2
What are the early signs and symptoms of macular degeneration?
In the early stages, you may not experience any symptoms at all. As the condition progresses, however, you may begin to notice the following changes in your vision:
- Blurry or distorted central vision, which can affect your ability to read, drive, or recognize faces.
- The need for brighter light when reading or doing close-up work.
- Difficulty adjusting to low light or seeing in dimly lit areas.
- A decrease in the intensity or brightness of colours.
- Straight lines that seem wavy or crooked.
It’s important to remember that these early symptoms of macular degeneration can be subtle and may not affect both eyes at the same time. If you notice any changes in your vision, no matter how small, it’s essential to schedule an eye exam with your doctor. Catching macular degeneration early is crucial for preserving your vision and preventing further vision loss.
Question 3
How quickly can macular degeneration progress after diagnosis?
Depending on type, severity and your individual circumstances, the progression of macular degeneration can vary. In some cases, macular degeneration can progress slowly over many years, while in other cases, it may progress more rapidly, within weeks.
While wet macular degeneration is generally considered the more serious and faster-progressing form of the condition, dry macular degeneration can also lead to significant vision loss, albeit at a slower pace.
It’s important to understand that the development of wet macular degeneration is always preceded by the dry form. Roughly 10-15% of cases of dry macular degeneration progress to the advanced and severe wet form.
This is why it’s important to be vigilant of any visual changes following a macular degeneration diagnosis. Here are some signs your macular degeneration may be getting worse:
- Your vision is blurrier or more distorted.
- You notice new blind spots or dark areas of your visual field.
- You take longer or find it more difficult to read or perform tasks that require detailed vision.
- The colours of familiar objects and places seem more dulled down than usual.
- When you turn a light switch on or off, you seem to need more time than usual to get adjusted to the new lighting.
If you notice any of these changes, and especially if you experience a sudden decrease in your visual acuity, it’s important to seek medical attention to assess the progression of your condition and determine whether it has developed into the wet form.
Catching changes early in your macular degeneration can minimise the risk of further vision loss and allow for more effective management of your condition.
Question 4
What are the treatment and management options available?
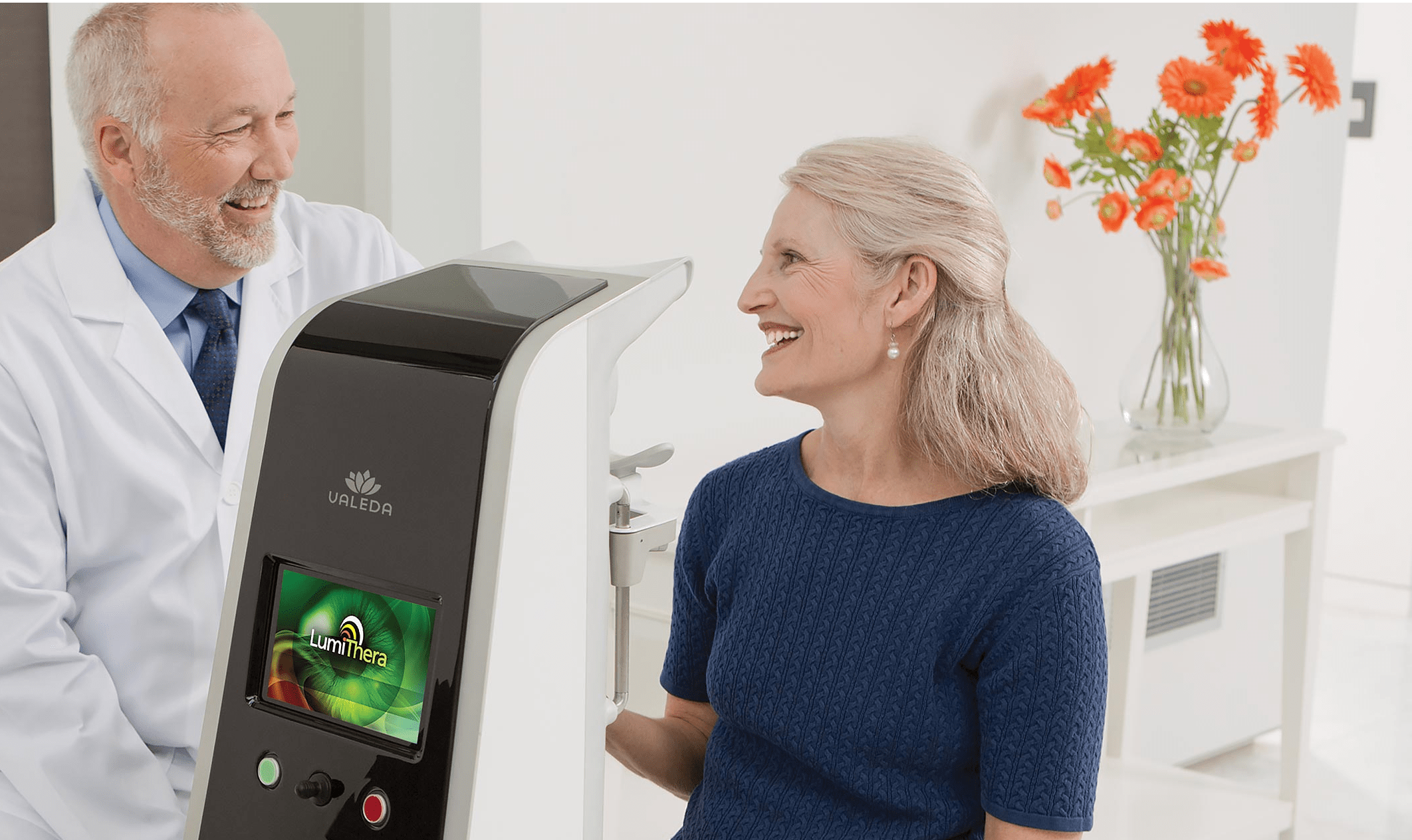
We offer treatment for both dry and wet macular degeneration, including a new technology by LumiThera that is the first approved treatment for dry macular degeneration.
-
Anti-VEGF injections.
For wet macular degeneration. In this type of form of the disease, abnormal blood vessels grow under the retina and leak fluid, as shown in the diagram below. The anti-VEGF medications work by blocking the activity of VEGF, which is responsible for the growth of these abnormal blood vessels.
During the injection procedure, the eye is numbed and the medication is directly injected into the centre of the eye. Anti-VEGF injections have been shown to be highly effective in improving and maintaining vision in many of our patients with wet macular degeneration.
-
Valeda Light Delivery System by LumiThera.
For dry macular degeneration, a special type of light therapy, called photoimodulation, is delivered to the retina. This light therapy helps to reduce inflammation and improve cellular metabolism in the retinal cells, which can slow the progression of the disease.
The treatment is painless and non-invasive, where a patient sits in front of the Valeda device and looks into the light for around 20 minutes, with multiple sessions over several weeks. Clinical studies have shown that this treatment can lead to statistically significant and long-term improvements in vision.
To slow down the progression of macular degeneration, it is crucial to make immediate lifestyle changes along with the treatment options mentioned earlier.
Question 5
Are there any lifestyle or dietary modifications that can help manage or prevent macular degeneration?
Although macular degeneration is primarily age-related, you can make adjustments to your daily routine that can help to manage or prevent it:
-
Eat a healthy diet.
Consuming a diet that is rich in fruits, vegetables, and fish, particularly those containing omega-3 fatty acids, reduce the risk of macular degeneration. Dark leafy greens such as spinach, kale, and collard greens are particularly good sources of antioxidants and nutrients that support eye health and help fight off disease.
-
Take nutritional supplements.
Certain vitamins and minerals, such as vitamins C and E, zinc, and copper, may help slow the progression of macular degeneration.
-
Maintain a healthy weight.
Obesity and a sedentary lifestyle have been linked to an increased risk of macular degeneration. Maintaining a healthy weight and being physically active can help to reduce the risk of the disease.
-
Don’t smoke.
Smoking is a major risk factor for macular degeneration. Quitting smoking or not starting in the first place will help to reduce the risk of the disease or slow its progression.
-
Protect your eyes.
Exposure to sunlight and blue light from electronic devices may contribute to the development of macular degeneration. Wearing sunglasses and blue light blocking glasses will reduce the amount of harmful light that reaches the eyes.
-
Regular eye exams.
Schedule regular eye exams to help detect early signs of macular degeneration, allowing for earlier intervention and treatment.
If you have any concerns about your vison or if you think you may be at risk of macular degeneration, speak with our specialist eyecare team. We are committed to managing and treating macular degeneration to preserve and maintain our patients’ vision. Our team of experts will work with you to develop the right strategy to navigate this often confusing and distressing diagnosis.
Remember, you don’t have to go through this alone.


 Eat a healthy diet.
Eat a healthy diet.