What is age-related macular degeneration?
Age-Related Macular Degeneration (AMD) is a degenerative eye disease that mainly affects those over 50.
The macula is a small area in your retina, in the back of your eye. It’s responsible for your central vision. As you age, changes in the macula can lead to inflammation and reduced function, gradually distorting central vision.
AMD doesn’t lead to total blindness, as peripheral vision is often unaffected. However, central vision loss associated with AMD can be severe. That’s why it’s essential to diagnose and treat AMD as early as possible to slow or stop its progression and preserve as much vision as possible.
Types of age-related macular degeneration
AMD comes in two types: wet and dry. Both forms present with the hallmark sign of AMD: Small, yellow deposits called drusen (depicted below) in the retinal layers.
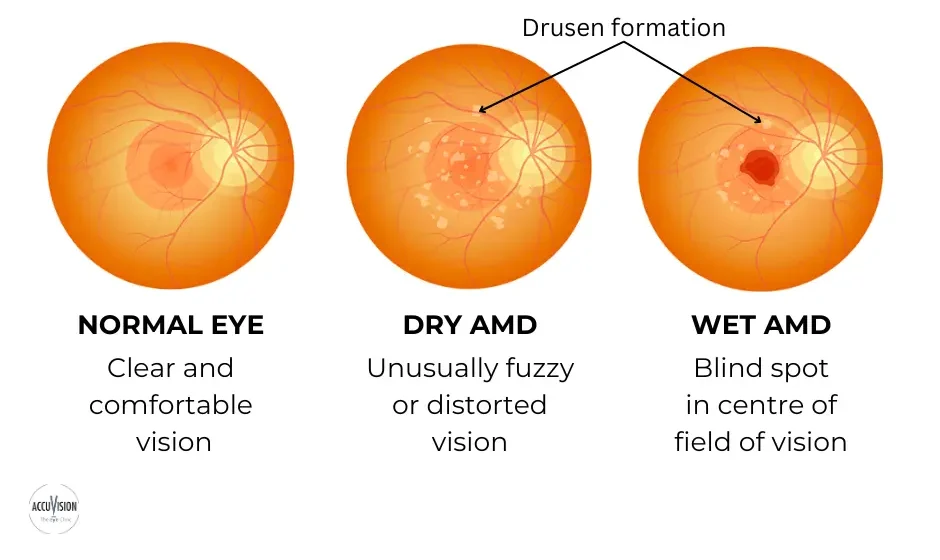
Dry AMD (Nonexudative AMD)
The most common form of AMD which makes up 80-85% of AMD cases.
Dry AMD occurs when parts of the macula break down as you age (most often the retinal photoreceptor cells and retinal pigment epithelium).
Over time, the accumulation of drusen deposits can cause reduced cell function and, if untreated, severe central vision loss.
Wet AMD (Exudative AMD)
Responsible for more than 80% of severe vision loss in AMD. Around 10-15% of dry AMD cases progress into wet AMD. Wet AMD occurs when abnormal blood vessels grow and leak under the macula, causing scarring and rapid central vision loss.Stages of age-related macular degeneration
Early AMD
Symptoms: Minimal or no symptoms
Treatment: Regular monitoring with eye assessments and supplements
Intermediate AMD
Symptoms: Gradual vision changes
Treatment:
Supplements, photobiomodulation
Advanced Dry AMD
Symptoms: Severe central vision loss
Treatment: Supplements, low vision aids, photobiomodulation
Advanced Wet AMD
Symptoms: Sudden and severe vision loss
Treatment: Anti-VEGF injections, laser therapy
Causes of age-related macular degeneration
Age-Related Macular Degeneration (AMD) is a complex eye condition with several factors contributing to its development:
Aging: As you age, your macular cells naturally weaken, making you more vulnerable to AMD.
History of AMD: If AMD runs in your family, your risk goes up, especially for the wet form of the condition.
Smoking: Smoking increases the chances of both dry and wet AMD.
Obesity: Increased body weight can cause higher inflammation and oxidative stress, and destabilise lipid levels. This can make drusen formation more likely.
Poor Diet: An unhealthy diet with too few essential nutrients and too much saturated fat can speed up AMD.
Inflammation: Certain inflammatory diseases can lead to the release of harmful proteins and chemicals that damage the macula.
While one can’t stop aging, you can make healthy choices, consider family history, and protect your eyes from harm to lower the chances of AMD or slow its progression as you age.
Symptoms of age-related macular degeneration

Being aware of early signs of AMD is vital so that you can seek early treatment and limit its progression. Here are the most common AMD symptoms:
Distorted Central Vision
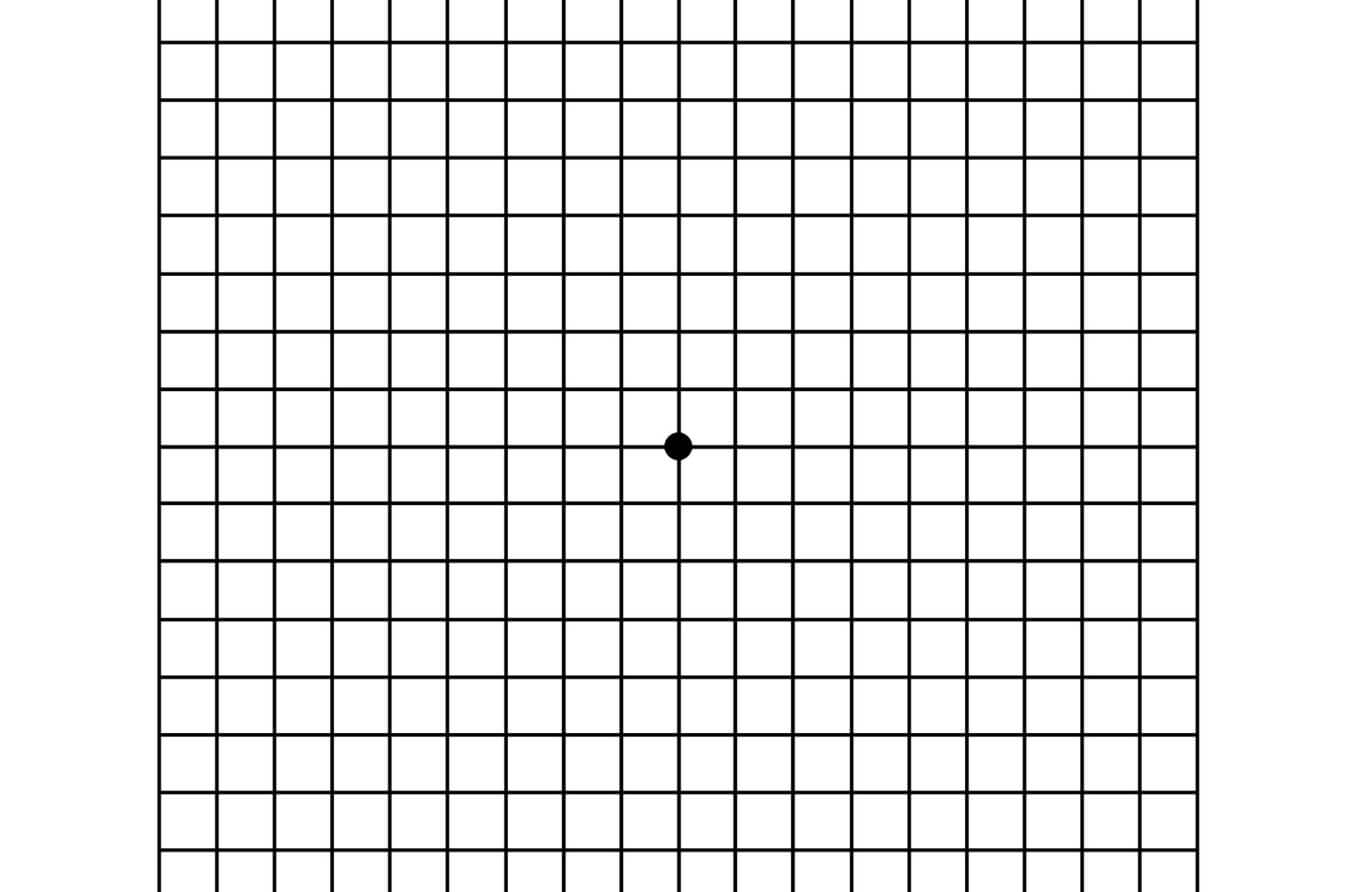
A hallmark early sign of AMD is the distortion of your central vision (shown by warped grid lines in image above).
Blind Spots or Dark Patches
AMD can create areas of dark blurriness in your central vision (shown as a central dark spot in image above).
Reduced Colour Perception
AMD may affect how you perceive colours; colours may seem less vibrant.
Light Sensitivity
AMD can cause sensitivity to bright light, causing discomfort and glare.
Difficulty Seeing in Low Light
Adapting to dim or low-light conditions can become challenging.
Symptoms can show up in one or both eyes, usually starting in one eye first.
Risks associated with age-related macular degeneration
If you or a family member has AMD or is at risk, it’s crucial to be aware of the wider implications it can have on overall health and well-being:
Difficulty With Detailed Tasks: AMD can cause central vision loss, making it hard to read, drive, or do detailed tasks.
Reduced Quality of Life: AMD can limit your ability to enjoy daily activities.
Emotional Challenges: AMD-related vision loss can lead to depression and anxiety.
Risk of Falls: Advanced AMD can affect balance, increasing the risk of falls and injuries.
Nutrition Issues: Vision problems may make it harder to purchase and prepare nutritious meals.
Medication Management: Vision loss might complicate managing medications and other health conditions.
Higher Healthcare Costs: Treating AMD and related issues can lead to more medical expenses.
Cognitive Function: Some research suggests a link between AMD and cognitive decline.
How to prevent age-related macular degeneration?
Incorporate the following practices into your daily routine to reduce the risk of AMD or slow its progression:
✓ Maintain a healthy weight.
✓ Eat a nutritious diet of fruit, veg, nuts & fish.
✓ Stay active with aerobic exercise.
✓ Wear UV protective sunglasses.
✓ Monitor blood pressure and sugar.
✓ Quit smoking.
✓ Limit alcohol intake.
✓ Get quality sleep.
✓ Schedule regular eye exams.
While these lifestyle changes will help, effective and accurate management of AMD requires professional clinical intervention.
Medical diagnosis of age-related macular degeneration
Early detection of Age-Related Macular Degeneration (AMD) is crucial because its initial signs can be subtle. Here are the ways an eye specialist will diagnose AMD:
You can perform this test at home to check if you have AMD or to monitor how your AMD is progressing. Here’s how:
Prepare Your Environment: Find a quiet, well-lit space. Wear your glasses (not varifocals or bifocals).
Close One Eye: Perform the test with one eye closed and repeat with the other eye.
Set Up the Grid: Keep the grid approximately 30 cm from your eyes.
Focus on the Grid: Stare at the dot in the centre of the grid.
Check for Abnormalities: Report any wavy lines or distortions.
- Monitor Changes: If you have already been diagnosed with AMD, keep track of your previous results and report any worsening distortions.
This imaging test reveals macular issues, especially for wet AMD. The image below shows how wet AMD can look in an OCT scan.

The scan on the left shows a front-on view and the right shows a cross-sectional view of the retina.
This OCT scan reveals a raised macula with big cysts around it, indicating fluid inside. Additionally, on the outer part of the retina, there’s a faint brightness in the OCT, indicating the growth of abnormal blood vessels.
We also use OCT to monitor response to therapy. We use it to monitor changes in thickness of the macula, detecting any fluid build up underneath the retina, or other retina problems.
This test helps eye specialists identify issues such as abnormal blood vessel growth.
For instance, in the centre of the fluorescein angiogram scan above, you can see a “network” of abnormal blood vessel growth from AMD.
This is standard vision chart comprises of 11 lines of block letters, starting with a large single letter at the top row. Its purpose is to assess your vision.
These eye drops widen your pupil so that we can have a more thorough look at your retina and macula.
Even without noticeable changes, routine eye check-ups can spot early AMD signs.
Consult an Eye Specialist for AMD if:
- You’re 50 or older with AMD risk factors.
- You see distortions in the centre of your vision.
- The Amsler Grid shows irregularities.
Don’t wait — timely eye check-ups can significantly affect AMD’s progression and your long-term vision quality.
Age-related macular degeneration treatment
Although there is no cure for AMD, the following treatment and management strategies can help slow its progression and preserve vision:
Dry AMD Treatment
Valeda Light Delivery System by LumiThera
LDS delivers specific light wavelengths to the retina. This aims to reduce inflammation and enhance the metabolism of the cells in your retina, slowing the progression of dry AMD and preserving vision.
Nutritional Supplements
A specific formulation of vitamins and minerals, known as the Age-Related Eye Disease Study (AREDS) formula, may be recommended to slow the progression of dry AMD. This formula includes antioxidants and zinc and may be provided under the guidance of your clinician.
Wet AMD Treatment
Anti-VEGF injections
Anti-VEGF medications work by blocking the activity of VEGF, a protein responsible for the growth of abnormal blood vessels seen in wet AMD. During this procedure, the eye is numbed and the medication is injected into the eye. Injections are repeated 4-6 weeks apart.
When deciding on anti-VEGF drugs like Eyelea®, Avastin®, and Lucentis®, a clinical trial by the National Institute of Health found similar performance in mild vision loss.
Eylea® may be more effective in conditions like diabetic macular edema, but Avastin® is notably more affordable.
Ultimately, your eye doctor’s advice, your individual response to treatment, and cost considerations play a role in choosing the best option for you.
Photodynamic Therapy (PDT)
PDT involves injecting a light-sensitive medication into the bloodstream, which is then activated by laser light. This process targets the blood vessels, helping to reduce leakage and minimise further damage to the macula.
Eye-Healthy Foods
Incorporate the following foods into your diet to slow progression or reduce the risk of AMD:
Spinach, kale, and collard greens contain protective antioxidants that safeguard your eyes (lutein and zeaxanthin).
Oranges, berries, and kiwi provide essential vitamin C which can prevent cellular damage by deactivating free radicals.
High in beta-carotene, which is then converted in the body into vitamin A — essential for good eye health.
Almonds, walnuts, and chia are antioxidant powerhouses, and contain essential vitamin E which has been shown to slow AMD progression.
Quinoa, brown rice, and oats provide nutrients (vitamin E, zinc, and niacin) for overall eye health.
Rich in lutein, zeaxanthin, and zinc, which help to protect your eyes.
Kidney beans, black-eyed peas, and lentils offer bioflavonoids and zinc which reduce AMD risk.
Especially red, orange, and yellow varieties contain vitamin C which has been shown to slow the progression of AMD.
What makes our AMD treatment unique?
Technology & Expertise
AMD Diagnosis Process by AccuVision Optometrist
At AccuVision, we use advanced diagnostics such as ultra-wide field retinal scanning and the latest 4D HD OCT to diagnose AMD.
We use two devices in tandem, the HeidelbergOCT and Optos, which have different modes, filters, and capabilities.
This in depth diagnosis process helps us customise your treatment with precision for the best vision possible.
Unique Treatment and Management for AMD
Our comprehensive AMD treatment includes:
- The proprietary Valeda Light Delivery System.
- Prescription of AREDS supplements when suitable.
- Anti-VEGF treatments for targeted therapy.
- Photodynamic therapy for non-invasive management.
- One-on-one lifestyle counselling to slow AMD progression and preserve vision.
What to Expect
What to Expect Before Treatment
You will receive a bespoke treatment plan optimised for your eyes and specific condition.
We encourage you to ask any questions you may have at this point so that you can go into your treatment comfortable and informed.
What to Expect During the Procedure
We guide you through each step of the treatment process, prioritising clear guidance and addressing any questions you may have.
Comprehensive Aftercare
Post-Procedure Short Term Care by AccuVision
After the procedure, short-term care is crucial. We prioritise your immediate recovery, closely monitoring your response immediately following your treatment.
We then provide detailed instructions for post-procedural care, including any necessary follow-up scheduling for monitoring or anti-VEGF treatments.
Post-Procedure Long Term Care by AccuVision
Recognising AMD as a long-term condition, our consultants develop customised long-term plans.
You will receive personalised treatment strategies based on natural changes, clinical indications, and your specific response to current treatment and management.
We help you schedule regular follow-ups to ensure sustained care and the best possible result. Our personalised care and 24/7 emergency line ensures that we are only ever a call away, should you need us.
Living with AMD: Before and after treatment
Living with Age-Related Macular Degeneration (AMD) can be challenging, but with advancements in diagnosis and treatment, patients often experience significant improvements in their quality of life.
Here’s how your life can change before vs after AMD treatment:
Before Treatment
❌ Visual Challenges: Blurred or distorted vision impacts daily activities like reading and recognising faces.
❌ Dependence: Advanced AMD may lead to increased reliance on others for tasks like shopping and cooking.
❌ Emotional Impact: Loss of central vision can result in emotional challenges such as depression or anxiety.
After Treatment
✓ Improved Vision: Successful treatment can slow progression of AMD, preserving and sometimes enhancing vision.
✓ Greater Independence: Improved vision fosters independence and self-sufficiency.
✓ Enhanced Emotional Well-being: Better vision often improves emotional health, reducing the psychological impact of AMD.
It’s crucial to diagnose and treat AMD during its early stages to slow progression and preserve as much vision as possible.
This is why regular visual assessments are crucial, especially as you get older. Regular follow-up care helps maintain and optimise treatment results for the best possible vision.
Frequently Asked Questions
Vision with macular degeneration typically appears as distorted spots in the central field of vision. These areas may also be darker or appear blurred. It may be challenging to read, recognise faces, or see fine details.
The below image is an approximation of the central vision loss and distortion that can occur with AMD.
The best treatment depends on the type of macular degeneration. For wet AMD, treatments like anti-VEGF injections are commonly used. For dry AMD, the Valeda Light Delivery System is a new treatment that aims to halt progression by breaking down drusen. Nutritional supplements and lifestyle changes are necessary for both dry and wet AMD.
Wet AMD is often treated with anti-VEGF injections, which can help reduce abnormal blood vessel growth and slow vision loss.
Dry AMD symptoms include blurred or distorted central vision, the need for brighter light when reading, and difficulty recognising faces.
Symptoms of wet AMD can include distorted or wavy vision, a sudden increase in the number of floaters, and dark spots in the central vision.
The progression varies among individuals. Some may experience gradual vision loss over several years, while others may lose vision more rapidly. Timely treatment can often slow the progression.
Early warning signs can include difficulty reading or seeing in low light, increased blurriness in central vision, and straight lines appearing wavy.
The first signs may include subtle changes in vision, such as difficulty reading small print, mild blurriness, or challenges with tasks that require detailed vision.
Macular degeneration is primarily caused by aging and genetic factors. Smoking, high blood pressure, and obesity can also increase the risk.
Currently, there is no cure for macular degeneration, but treatments can help manage the condition and slow its progression.
The duration varies widely among individuals. Some may never go completely blind, while others may experience severe vision loss more rapidly. Early diagnosis and treatment can make a significant difference in preserving vision.